Reverse Insulin Resistance, Regenerate β-Cells & Treat Complications by Stem Cell Therapy— Without Lifelong Medication Dependence
Autologous Adipose-Derived Mesenchymal Stem Cell (ADMSC) Therapy | 100–200 Million Cultured Cells | Government-Certified Quality | Cell Grand Clinic, Osaka
- Why Medication Alone Is Not Enough: The Real Problem with Conventional Diabetes Treatment
- Medication vs. Stem Cell Therapy: A Fundamentally Different Approach
- The Biggest Advantage Of Stem Cell Treatment : Treating Complications, Not Just Blood Sugar
- Clinical Evidence Of Stem Cell Treatment For Diabetes: What Published Research Shows
- Why Adipose-Derived Stem Cells Are Superior
- Why Japan? The World’s Strictest Regulatory Framework
- Why Cell Grand Clinic? Our “Fresh, Pure, Young” Quality Standard
- Treatment Protocol: What to Expect
- Addressing the Skepticism: Is Stem Cell Therapy Proven Enough?
- Frequently Asked Questions
- Take Control: From Symptom Management to Regeneration
Why Medication Alone Is Not Enough: The Real Problem with Conventional Diabetes Treatment
If you are living with Type 1 or Type 2 Diabetes, you already know the daily reality: metformin, sulfonylureas, GLP-1 receptor agonists, SGLT2 inhibitors, or insulin injections. You monitor your blood sugar, adjust your doses, and follow the routine.
But here is the uncomfortable truth that your physician may not fully explain: every one of these medications manages your blood sugar — none of them repairs the damage that is causing your diabetes.
According to the International Diabetes Federation, over 537 million adults worldwide are living with diabetes, projected to reach 643 million by 2030. Despite decades of pharmaceutical development, the fundamental limitation remains unchanged: oral and injectable medications control glucose levels on the surface while the underlying destruction continues silently beneath.
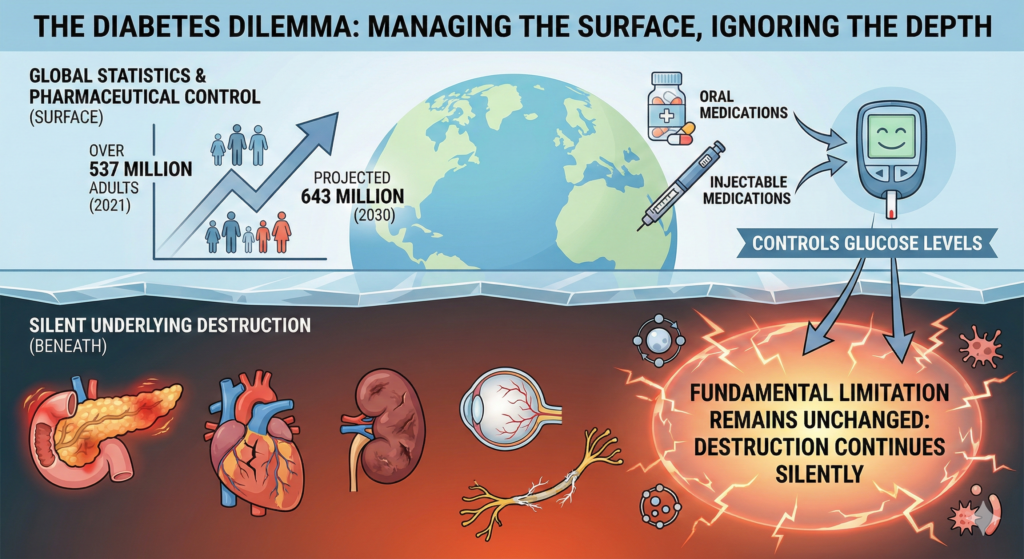
What conventional medications cannot do:
They cannot regenerate your pancreatic β-cells — the insulin-producing cells that are being destroyed or exhausted. They cannot reverse insulin resistance at the cellular level — where your muscles, liver, and fat tissue have stopped responding to insulin. They cannot repair your damaged blood vessels — meaning the complications (kidney disease, retinopathy, neuropathy, erectile dysfunction) continue to progress even when your HbA1c looks acceptable. And they cannot address the chronic inflammation that drives the disease forward year after year.
This is why 70–90% of β-cell function is already compromised by the time Type 2 Diabetes is diagnosed. This is why 14–25% of Type 2 patients eventually require insulin injections because oral medications fail. And this is why diabetic complications — blindness, amputation, kidney failure — continue to claim lives even among patients who diligently follow their medication regimens.
The question is not whether your medication is working. The question is whether managing symptoms is enough — or whether you deserve a treatment that targets the root causes of your disease.
Medication vs. Stem Cell Therapy: A Fundamentally Different Approach
To understand why stem cell therapy represents a paradigm shift, consider what happens at the cellular level with each approach.
What Oral Medications Do
Metformin reduces hepatic glucose output and improves insulin sensitivity slightly. Sulfonylureas force your remaining β-cells to produce more insulin — accelerating their exhaustion. GLP-1 receptor agonists slow gastric emptying and enhance insulin secretion. SGLT2 inhibitors cause your kidneys to excrete excess glucose through urine. Insulin injections simply replace what your body can no longer produce.
Every single mechanism above works downstream of the actual problem. They compensate. They mask. They manage. Not one of them heals.
And critically, they must be taken daily — for the rest of your life. Miss a dose, and your blood sugar spikes. Stop the medication entirely, and your condition returns immediately — often worse than before, because the underlying disease has continued to progress during the years of “management.”
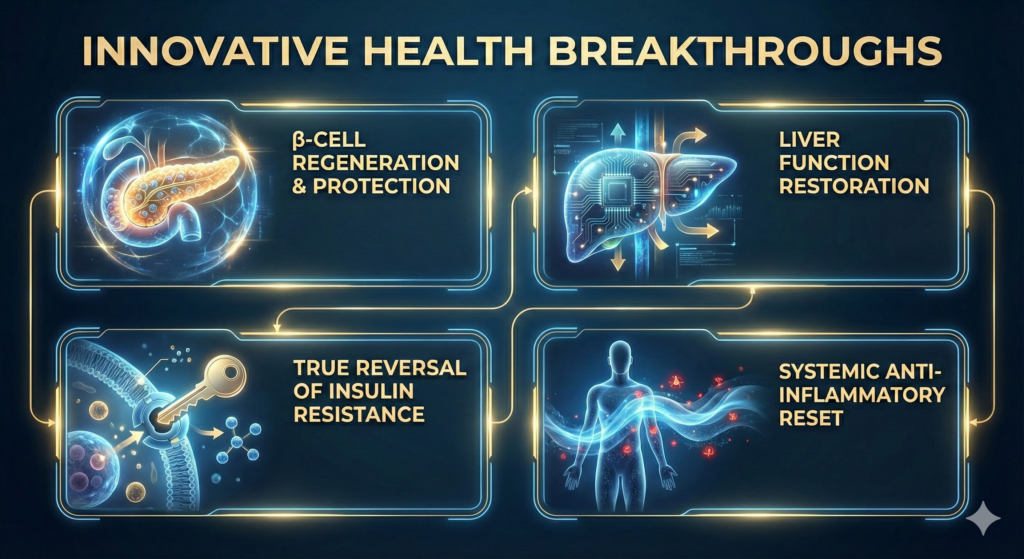
What Stem Cell Therapy Does
Autologous Adipose-Derived Mesenchymal Stem Cell (ADMSC) therapy works through an entirely different paradigm. Instead of compensating for damage, it activates your body’s own repair mechanisms across multiple pathways simultaneously.
Published research in The Journal of Clinical Endocrinology & Metabolism (2023) and Stem Cells International (2022) has demonstrated that ADMSCs combat diabetes through four distinct mechanisms that no medication can replicate:
1. β-Cell Regeneration and Protection
Your stem cells release powerful growth factors (VEGF, TGF-β, IGF-1, HGF) that stimulate your pancreas to regenerate insulin-producing β-cells. Simultaneously, they protect existing β-cells from further destruction by reducing oxidative stress and inflammatory cell death. In laboratory studies, islets treated with ADMSCs showed dramatically reduced cell death — just 1–3% loss compared to 22% without stem cell support.
For Type 1 Diabetes patients specifically, ADMSCs halt the autoimmune attack on β-cells by modulating the immune system’s misdirected response.
2. True Reversal of Insulin Resistance
Unlike metformin, which modestly improves insulin sensitivity through a single pathway, stem cell therapy addresses insulin resistance at multiple molecular targets. ADMSCs increase GLUT4 expression — the glucose transporters in your liver, muscles, and fat tissue. They restore the IRS-1/AKT signaling pathway, which is the primary mechanism through which insulin communicates with your cells. They suppress the NLRP3 inflammasome — a key inflammatory trigger that blocks insulin signaling. This is not partial improvement. This is restoration of the cellular machinery that makes insulin work properly.
3. Liver Function Restoration
Your liver is central to glucose regulation, and in diabetes, hepatic dysfunction drives both fasting and post-meal blood sugar spikes. MSC therapy has been shown to improve liver function markers (ALT, AST), reduce hepatic fat accumulation, and promote glycogen synthesis — lowering blood glucose within 24 hours of treatment.
4. Systemic Anti-Inflammatory Reset
Chronic low-grade inflammation is now recognized as a primary driver of both Type 1 and Type 2 Diabetes. ADMSCs convert pro-inflammatory M1 macrophages into anti-inflammatory M2 macrophages, expand regulatory T cells for sustained immune balance, and shift the entire cytokine profile from destructive to protective. This is a system-wide inflammatory reset that no single medication can achieve.
➤ Book Your Private Consultation
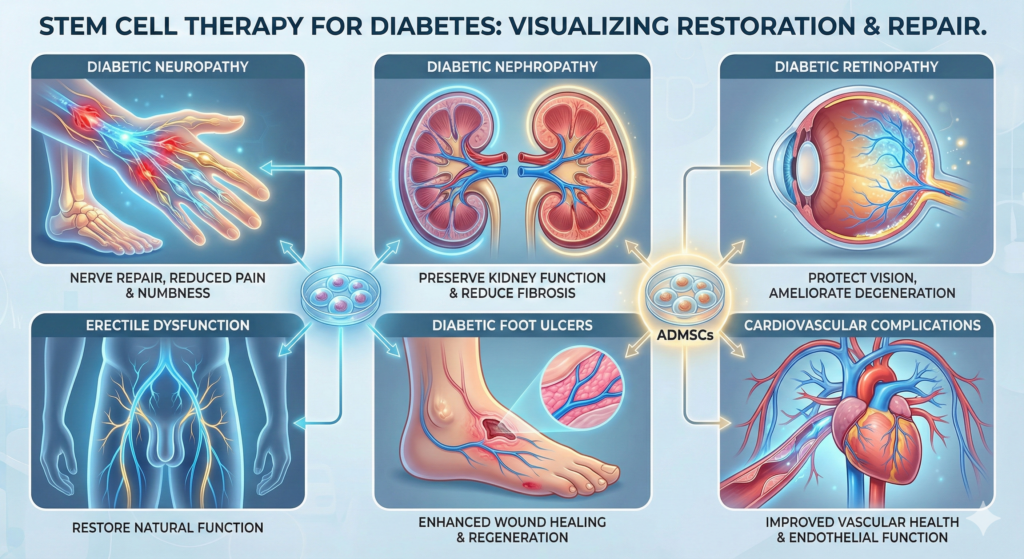
The Biggest Advantage Of Stem Cell Treatment : Treating Complications, Not Just Blood Sugar
This is the critical difference that separates stem cell therapy from every pharmaceutical approach available today.
Diabetic complications — neuropathy, nephropathy, retinopathy, erectile dysfunction, cardiovascular disease, foot ulcers — are all fundamentally vascular diseases. They occur because diabetes damages the small blood vessels and nerves throughout your body.
No oral diabetes medication treats these complications directly. They can only attempt to slow progression by controlling blood sugar. But even with perfect glucose control, many patients still develop complications because the vascular damage has its own momentum.
ADMSC therapy is, by its nature, a systemic vascular treatment. A 2024 review published in Diabetes, Obesity and Metabolism specifically evaluated ADMSCs for diabetic complications and documented significant benefits:
Diabetic Neuropathy
Stem cells promote nerve repair and angiogenesis (new blood vessel formation), reducing numbness and pain in the extremities — symptoms that medication cannot address.
Diabetic Nephropathy (Kidney Disease)
ADMSCs repair the endothelial lining of kidney blood vessels and reduce fibrosis, helping to preserve kidney function that would otherwise decline irreversibly.
Diabetic Retinopathy
Through anti-inflammatory and pro-angiogenic effects, ADMSCs ameliorate retinal degeneration — protecting your vision.
Erectile Dysfunction
Improved microcirculation and nerve function restores natural function — a result that PDE5 inhibitors (like Viagra) can only temporarily simulate.
Diabetic Foot Ulcers
Enhanced wound healing through tissue regeneration and new blood vessel formation — directly addressing the condition that leads to amputation.
Cardiovascular Complications
Improved endothelial function and reduced vascular inflammation — the most common cause of death in diabetic patients.
When you take metformin, you are controlling a number. When you receive stem cell therapy, you are repairing the system.
Clinical Evidence Of Stem Cell Treatment For Diabetes: What Published Research Shows
This is not theoretical. Published clinical trials have documented measurable outcomes.
Type 1 Diabetes Results
Research published in The Journal of Clinical Endocrinology & Metabolism (2023) documented patients with recent-onset T1DM receiving ADMSCs who achieved: insulin requirement reduction from 0.61 to 0.22 IU/kg (a 64% decrease), HbA1c improvement from 7.48% to 6.47%, and increased C-peptide levels indicating improved β-cell function.
Long-term follow-up (mean 31.71 months) showed sustained improvement: C-peptide increased from 0.22 to 0.92 ng/mL, HbA1c decreased from 10.99% to 6.72%, and daily insulin requirements dropped from 64 to 39 IU.
Type 2 Diabetes Results
A comprehensive review published in Stem Cells International (2022) confirmed that MSC therapy in T2DM patients produces measurable improvements in HbA1c, fasting glucose, C-peptide levels, and insulin resistance markers — with benefits sustained over 12 months and beyond.
A 2024 meta-analysis published in Frontiers in Endocrinology, analyzing data across multiple clinical trials, concluded that mesenchymal stem cell therapy shows consistent therapeutic potential for diabetes management. Importantly, the analysis found that adipose-derived MSCs showed particularly strong outcomes for treating diabetic complications including neuropathy and nephropathy — a finding that underscores the systemic vascular benefits of this approach.
Why Adipose-Derived Stem Cells Are Superior
Not all stem cells are equal. Cell Grand Clinic exclusively uses adipose-derived (fat-derived) mesenchymal stem cells for several evidence-based reasons:
100–500× greater cell yield than bone marrow: Adipose tissue contains dramatically more stem cells per gram, enabling therapeutic doses with minimal tissue harvest.
Minimally invasive harvesting: Unlike bone marrow aspiration (which requires needle insertion into the hip bone under general anesthesia), adipose tissue collection uses a simple mini-liposuction under local anesthesia. You return to your hotel immediately.
Superior biological properties: Published comparative studies demonstrate that ADMSCs exhibit enhanced proliferation capacity, greater genetic stability, lower immunogenicity, and higher immunomodulatory capacity than bone marrow-derived stem cells.
No ethical concerns: Using your own cells eliminates ethical issues associated with embryonic stem cells and virtually eliminates rejection risk.
Why Japan? The World’s Strictest Regulatory Framework
In the global landscape of regenerative medicine, Japan occupies a unique position. It is the only major country with comprehensive legislation — the Act on the Safety of Regenerative Medicine (2014) — specifically designed to regulate stem cell treatments while enabling clinical innovation.
This matters enormously for international patients because it means: every treatment plan must be reviewed and approved by certified government regenerative medicine committees. All cells must be cultured in licensed Cell Processing Centers (CPCs) meeting pharmaceutical-grade GMP standards. Adverse events are mandatorily reported to a national database. Ongoing safety surveillance with regular inspections ensures consistent quality.
Many countries offering stem cell therapy operate in regulatory gray zones. Japan’s framework ensures that when you receive treatment, the quality, safety, and oversight meet the highest standards in the world.
Why Cell Grand Clinic? Our “Fresh, Pure, Young” Quality Standard
At Cell Grand Clinic, we do not administer raw, uncounted cell isolates. Every treatment involves cells cultured at our government-certified Cell Processing Center to achieve the therapeutic concentrations required for clinical efficacy.
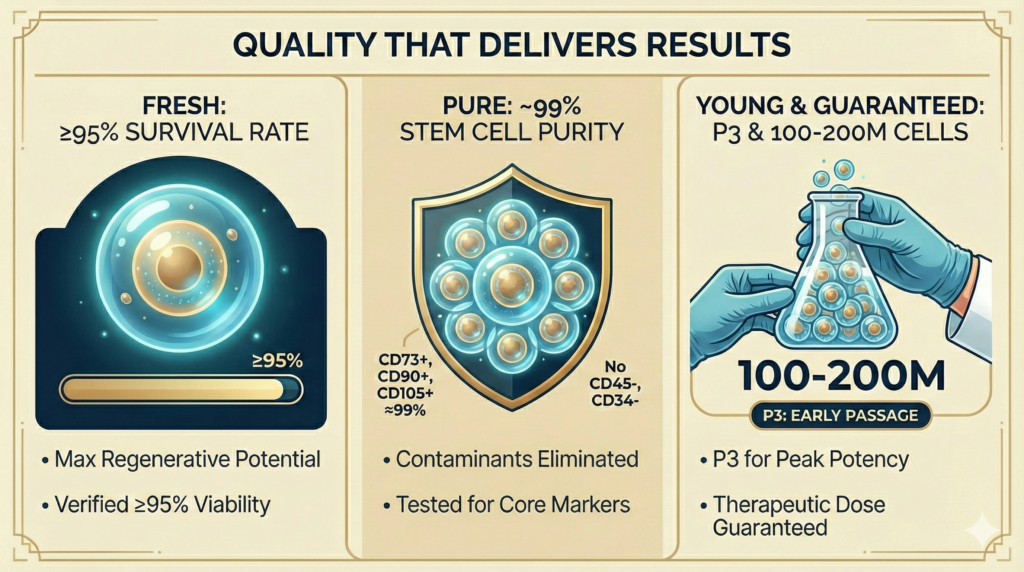
FRESH: Cell Viability: ≥98% (verified before every administration). Cells are processed and administered within optimal timeframes to maximize viability and therapeutic potential.
PURE: Multi-marker surface antigen screening (CD73+, CD90+, CD105+; CD45–, CD34–) ensures near-100% purity.
YOUNG: We use low-passage cells (P3), which retain full regenerative capacity. Many clinics use high-passage cells (P5+) with significantly diminished therapeutic effects.
Our Quality Metrics vs. Industry Standards
Cell Viability: ≥98% (verified before every administration) vs. industry average of 70–85%.
Cell Purity: Near 100% with rigorous multi-marker screening.
Cell Passage: P3 with 200 million cells — preserving maximum regenerative potency.
▶More information about stem cell
Government Certifications
MHLW Authorization (Ministry of Health, Labour and Welfare approved protocols). Regenerative Medicine Class II classification (highest category for outpatient stem cell procedures). 10 Type II Government Licenses for regenerative medicine. Government-certified CPC (FA5250001). ABRM-Certified Physician (American Board of Regenerative Medicine diplomate).
➤ Book Your Private Consultation
Treatment Protocol: What to Expect
For Diabetes Patients
Systemic IV Drip: 100–200 million MSCs via intravenous infusion (60–90 minutes) targeting T1DM/T2DM and systemic complications.
Local Injection: Customized dosing for targeted conditions such as diabetic erectile dysfunction.
Combination Therapy: IV + local injection for comprehensive treatment.
Timeline for International Patients
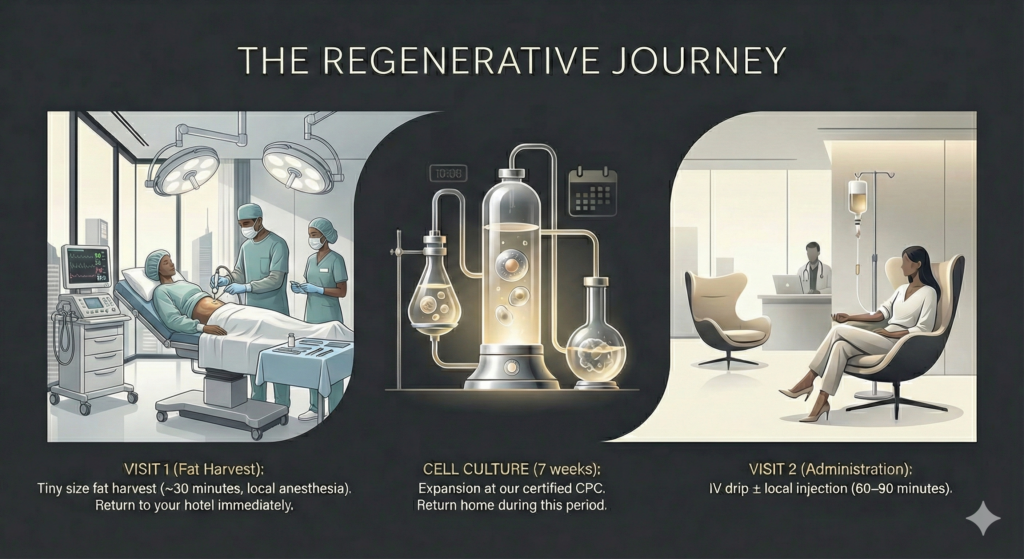
Step 1 — Online Consultation: Remote screening, medical record review, personalized treatment planning.
Step 2 — Visit 1 (Fat Harvest): Tiny size fat harvest (~30 minutes, local anesthesia). Return to your hotel immediately.
Step 3 — Cell Culture (7 weeks): Expansion at our certified CPC. Return home during this period.
Step 4 — Visit 2 (Administration): IV drip ± local injection (60–90 minutes).
Total time in Japan: approximately 2–3 days per visit.
Expected Timeline of Results
At 1–3 months: Initial improvements in glucose levels and neuropathy symptoms
At 3–6 months: Measurable HbA1c reduction and C-peptide increase
After 6months: Sustained effects and potential medication reduction under physician supervision.
Addressing the Skepticism: Is Stem Cell Therapy Proven Enough?
We believe in transparency. Some physicians and researchers raise legitimate concerns about stem cell therapy for diabetes, and you deserve to hear them — along with our response.
“The evidence is still limited to small clinical trials.”
This is partially true. Most published trials involve dozens, not thousands, of patients. However, the consistency of positive outcomes across multiple independent research groups — spanning China, Brazil, the Middle East, and Europe — makes the evidence compelling. A 2024 meta-analysis in Frontiers in Endocrinology pooled data from multiple trials and confirmed statistically significant improvements in glycemic control. Moreover, over 143 clinical trials for stem cell diabetes therapy have been registered globally, with mesenchymal stem cells representing 52.4% of all trials. The field is moving rapidly from early-phase trials to larger confirmatory studies.
“Results vary between patients.”
This is true of every medical intervention, including conventional medications. However, the key difference is what you are gaining: conventional medications guarantee lifelong dependence with zero possibility of disease reversal. Stem cell therapy offers the possibility of actual biological repair — reduced medication dependence, improved β-cell function, and treatment of complications — with a safety profile that 15 years of meta-analysis data has confirmed as excellent.
“Why not just use the newer GLP-1 drugs like Ozempic or Mounjaro?”
GLP-1 receptor agonists and dual GIP/GLP-1 agonists represent genuine pharmaceutical advances. They improve glucose control, promote weight loss, and may have cardiovascular benefits. But they share the same fundamental limitation as all medications: they do not repair β-cells, they do not reverse vascular damage, they do not treat neuropathy or nephropathy, and they require continuous use. The moment you stop taking them, the benefits disappear. Stem cell therapy, by contrast, aims to create lasting biological change — regenerated tissue and restored function that persists after the treatment.
For many patients, the optimal approach may be combining pharmaceutical management with regenerative therapy — using medications to maintain control while stem cells work to repair the underlying damage.
Frequently Asked Questions
Can stem cell therapy cure my diabetes?
We do not use the word “cure.” What clinical evidence demonstrates is that many patients achieve clinical remission — where blood sugar stabilizes to the point where medication can be significantly reduced or paused under physician supervision. The degree of improvement depends on your disease duration, remaining β-cell function, severity of insulin resistance, existing complications, and overall metabolic health.
Is this treatment safe?
Autologous ADMSC therapy has an excellent safety profile. Because we use your own cells, there is no immune rejection risk. A comprehensive 15-year meta-analysis published in Stem Cell Research & Therapy (2021) found no increased cancer risk associated with MSC therapy. Japan’s regulatory framework adds an additional layer of safety assurance unmatched globally.
I am worried about complications like blindness or amputation. Can this help?
Yes. One of the most significant benefits of ADMSC therapy is angiogenesis — the formation of new blood vessels. By restoring microcirculation to the eyes, kidneys, nerves, and extremities, stem cell therapy directly opposes the vascular deterioration that leads to these devastating complications. This is something no oral medication can do.
Do you treat both Type 1 and Type 2 Diabetes?
Yes. For T1DM, ADMSCs halt autoimmune destruction and protect remaining β-cells. For T2DM, the focus is on reversing insulin resistance, reducing systemic inflammation, and regenerating β-cell function. Both types benefit substantially from treatment of diabetic complications.
Take Control: From Symptom Management to Regeneration
You have spent years managing your diabetes with medication. The numbers may look acceptable on paper. But if you are honest with yourself, you know the disease is progressing. The complications are advancing. The medication doses are increasing.
There is another path — one that does not replace your medications overnight, but offers something no pill or injection ever could: the opportunity to repair the damage, restore function, and potentially reduce your dependence on lifelong pharmaceutical management.
Stem cell therapy is not about abandoning conventional medicine. It is about adding a regenerative dimension to your treatment — one that works to heal the underlying disease rather than merely suppress its symptoms. This is the future of diabetes care, and it is available today under the strictest regulatory oversight in the world.
At Cell Grand Clinic in Osaka, Japan, we provide personalized stem cell therapy for international patients who are ready to move beyond management — toward regeneration.
➤ Book Your Private Consultation
📍 Location: Shinsaibashi, Osaka, Japan
🌐 Languages: English, Japanese, Chinese
✈️ Nearest Airport: Kansai International Airport (KIX)
🏥 10 Type II Government Licenses | ABRM-Certified Physician | Government-Certified CPC
References
5. Nguyen A, et al. Adipose tissue stem cells for therapy. J Clin Med. 2020;9(6):1925.
8. International Diabetes Federation. IDF Diabetes Atlas. 10th ed. 2021.
Last Updated: February 2026
Disclaimer: Individual results may vary. This information is for educational purposes and does not constitute medical advice. Stem cell therapy outcomes depend on individual health conditions, disease severity, remaining β-cell function, and other factors. Always consult with a qualified healthcare provider before making treatment decisions. Cell Grand Clinic operates under Japan’s Act on the Safety of Regenerative Medicine with all required government authorizations.